Osteoarthritis causes the degeneration, or breakdown, of the structural components of a joint. The degenerative process may involve fibrocartilage, articular cartilage and bone. Having discussed the importance that fibrocartilage plays in certain joints in prior articles, here we will discuss articular cartilage, the causes for its degeneration and treatment options.
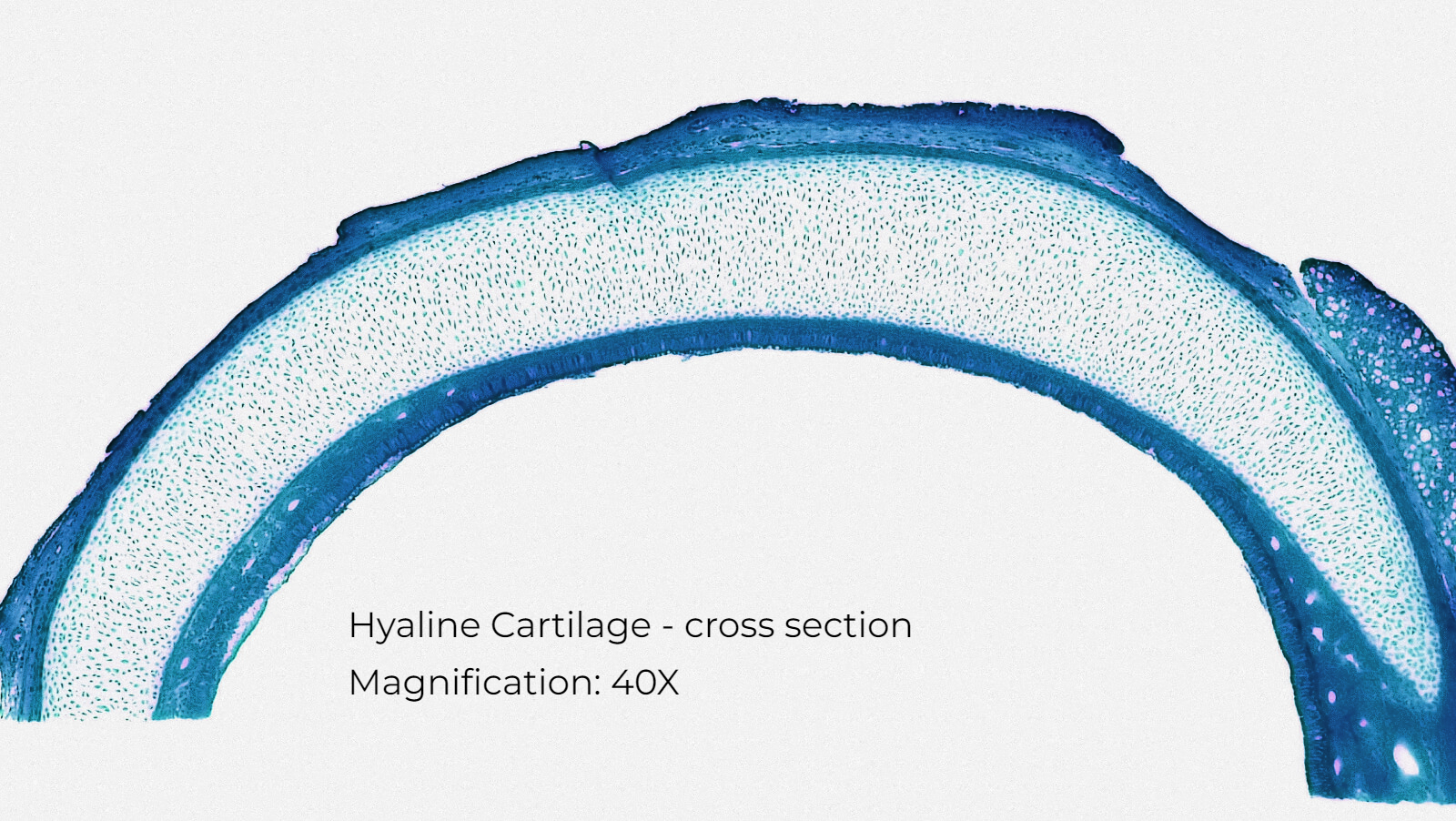
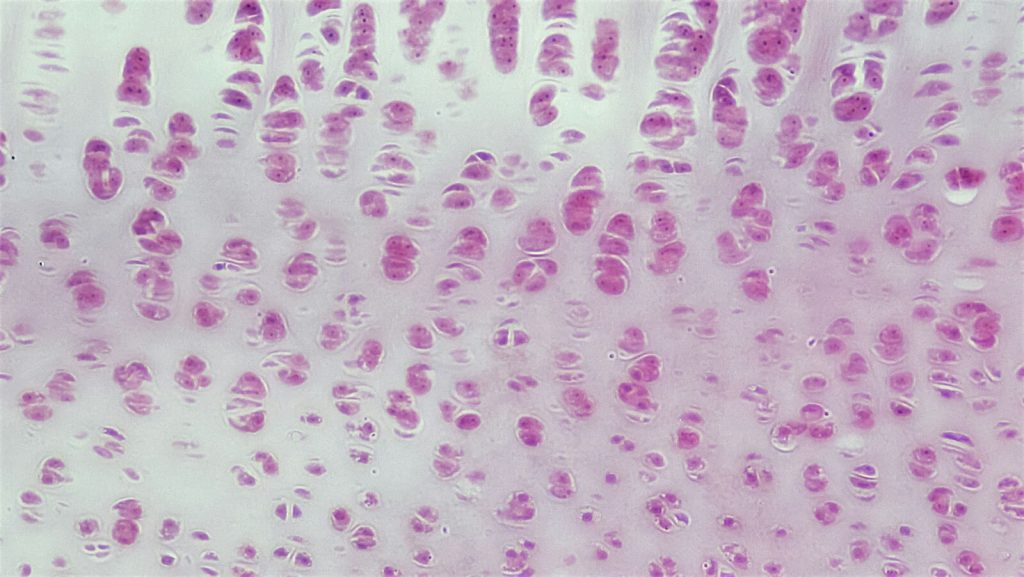
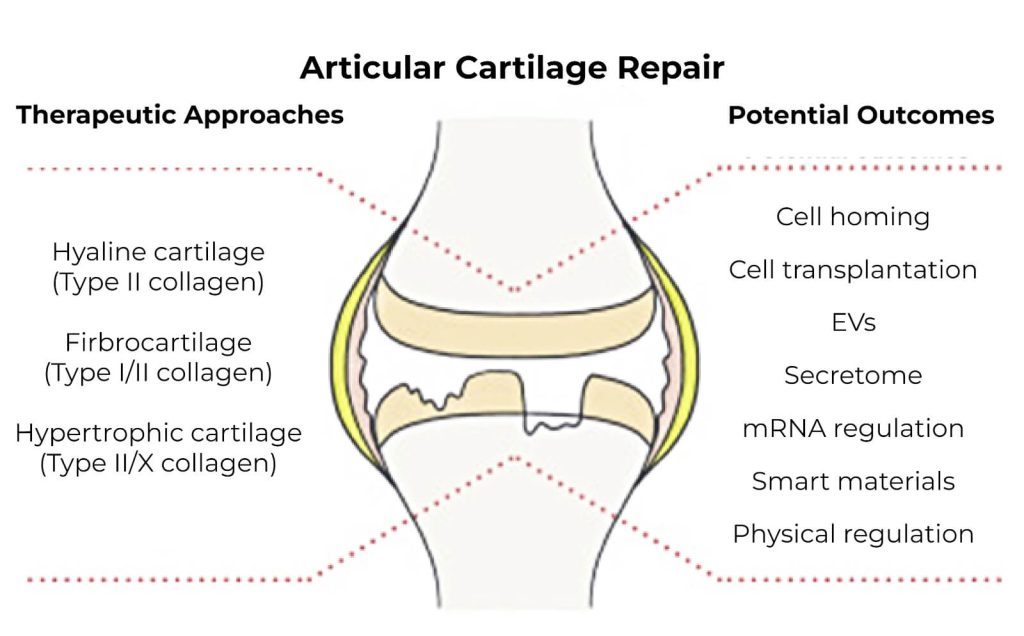
Articular cartilage, or hyaline cartilage, is a layer of collagen that lines the ends of the bones. The cartilage is composed of 60-85% water, type II collagen and extracellular matrix (ECM). The ECM and collagen provide hydration, lubrication, strength and a smooth surface to the bone ends. The thickness of the articular cartilage varies from joint to joint, averaging between 1 to 4.4mm depending on the joint. Weight bearing joints like the hip and knee have more hyaline cartilage than non-weight bearing joints like the head of the humerus where it meets the shoulder.1,2 Some joints, including the knee, hip, shoulder and temporomandibular joint, also have fibrocartilage. Fibrocartilage provides greater protection against compressive forces. The knee meniscus and shoulder labrum are examples of fibrocartilage.
The causes for joint articular cartilage damage
Acute damage to articular cartilage is often caused from a sports injury. Such injuries are caused by torsional joint loading with repetitive impact, in other words a repetitive, twisting motion combined with the force of one’s body weight.3 Damage can be limited to the articular surface, the subchondral bone (the bone under the articular cartilage), or to both the cartilage and the subchondral bone3. Very soon after an injury, collagen cells called chondrocytes begin apoptosis, or cell death. This is coupled with the release of inflammatory mediators (chemicals) into the local area, causing further damage to the articular cartilage (fig 1). This cellular death may last up to 48 hours following the injury.4 Disconcertingly, such damage to the articular cartilage can predispose a joint to developing osteoarthritis even when osteoarthritis had not previously been present. Malalignment, repetitive use and inflammatory conditions such as osteoarthritis and rheumatoid arthritis are other causes for articular damage.
Non-surgical Treatment Solution
Articular cartilage is avascular, meaning it lacks its own blood supply. This is why the body cannot repair such damage on its own and requires intervention. Adipose derived mesenchymal stem cells, when injected into joints with articular damage, can differentiate into cartilage. After the stem cells are injected into a joint, they find their target through a process known as stem cell “homing” effect. They adhere to the target surface and begin the regeneration of cartilage, filling in breaks in the smooth cartilage.5 For the longevity of a joint, it is important that proper alignment of a joint is achieved. To develop proper joint alignment and preserve the gains achieved by stem cell treatment, physical therapy guidance and exercises are often critical to begin strengthening and engaging the correct muscles when performing everyday movements such as walking.
Dr. Stacey Guggino, ND, LAc, graduated from the National College of Natural Medicine in Portland, Oregon with a Doctorate in Naturopathy and a master’s degree in Oriental Medicine. For the past 12 years, she has specialized in treating pain and sports injuries with acupuncture and prolotherapy. Dr. Guggino has also studied and practiced aesthetic medicine for 11 years.
Sources
- Shah RF, Martinez AM, Pedoia V, Majumdar S, Vail TP, Bini SA. Variation in the Thickness of Knee Cartilage. The Use of a Novel Machine Learning Algorithm for Cartilage Segmentation of Magnetic Resonance Images. J Arthroplasty. 2019 Oct;34.
- Schleich C, Bittersohl B, Antoch G, Krauspe R, Zilkens C, Kircher J. Thickness Distribution of Glenohumeral Joint Cartilage. Cartilage. 2017 Apr;8(2):105-111
- Buckwalter JA. Articular cartilage injuries. Clin Orthop Relat Res. 2002 Sep;(402):21-37.
- Jhase Sniderman, Patrick Henry. Articular reductions – how close is close enough? A narrative review. Injury. Volume 51, Supplement 2, 2020,Pages S77-S82
- Pak J, Lee JH, Pak N, Pak Y, Park KS, Jeon JH, Jeong BC, Lee SH. Cartilage Regeneration in Humans with Adipose Tissue-Derived Stem Cells and Adipose Stromal Vascular Fraction Cells: Updated Status. Int J Mol Sci. 2018 Jul 23;19(7).
Photos by Fayette Reynolds on Unsplash and Flickr