Recently, a friend told me that he didn’t feel comfortable going skiing anymore because of a meniscus tear that happened three months ago. His current management of his knee consists of limiting most of his activity, intermittently taking ibuprofen and “living with it“ because he didn’t know what else to do. Sadly, my friend is not alone in being unaware of supportive alternatives for his injury.
An overview of an unrepaired meniscus and the knee joint
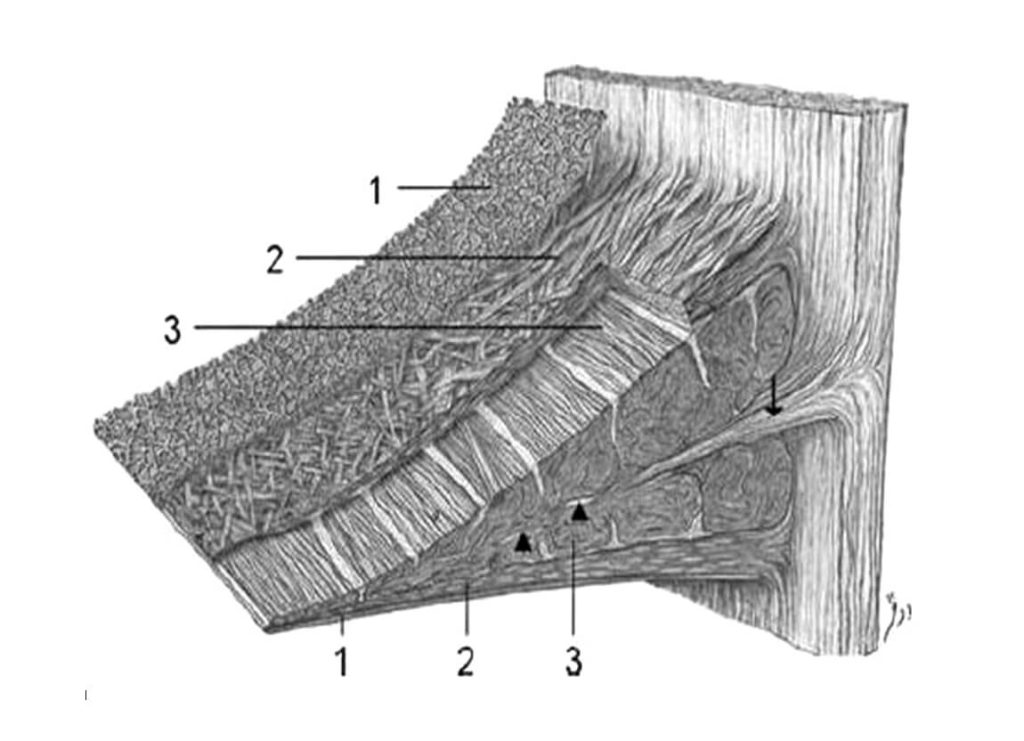
Whether the result of injury or degenerative microtears that develop as we age, meniscal tears contribute to the development of an osteoarthritic knee. The meniscus consists of 75% Type I collagen. Collagen and other molecules that attract water make up the extracellular matrix (“ECM”) of the meniscus. This ECM provides the meniscus with lubrication and the capacity for it to withstand continual load-bearing1. The collagen is akin to a layered woven structure (see illustration below). This woven structure transfers the compressive load of the body’s mass to the entire meniscus, rather than isolating the load to one area. The meniscus also protects cartilage on the femur and tibia, the bones in the hinge-like joint of the knee.
With an injury to the meniscus, there is a biochemical shift in the composition of the ECM from one that was once supportive to one that is inflamed or degraded. With prolonged inflammation of the ECM, the meniscus becomes weakened and thin. More severe tears of the meniscus, known as radial tears, are likely to ensue. Meniscal migration or movement beyond where the femur and tibia meet, also called meniscal extrusion, occurs with an unrepaired meniscus2. With the meniscus weakened and shifted, the articular cartilage that lines the bones becomes affected. Soon bony growths known as osteophytes develop on both the femur and tibia as the articular cartilage becomes thinner. The knee joint is now moderately to severely osteoarthritic.
Osteoarthritis of the Knee
Osteoarthritis (“OA”) of the knee can also occur independently of a meniscal tear. Risk factors for osteoarthritis include obesity, genetics, being female, living past the age of 50, and structural abnormalities. While it has long been recognized that untreated meniscal abnormalities can lead to OA, researchers also observe that the opposite holds true: An osteoarthritic knee can lead to meniscus tears.
In a 2021 study, the researchers compared the load bearing ability of a normal knee’s meniscus with that of a meniscus of an osteoarthritic knee. The researchers concluded that, due to the degenerative process in the joint – reduced hyaline cartilage, joint narrowing and malalignment – there is a reduction in the tensile strength of the meniscus, causing the meniscus to stiffen. Naturally, the stiffening makes the meniscus less compressible under load. As a result, there is a more concentrated area of stress in the posterior medial parts of the inner meniscus3. This finding correlates well with what we see clinically: radial tears of the posterior medial meniscus horn are common both with injuries and in patients suffering from OA.

Therapies to repair your meniscus
In the last twenty years, at Oregon Regenerative Medicine we have witnessed the success of our therapies in repairing trauma related tears, degenerative tears and osteoarthritis. We perform on-site ultrasound examinations to determine peripheral meniscal tears, meniscal extrusion, narrowing of the joint space and the extent of osteophytic growth. This assists us in determining whether platelet rich plasma or adipose derived mesenchymal stem cell therapy would be most appropriate for your knee. These therapies neutralize inflammation and concentrate the joint with reparative cells to heal the injury. Initiating the therapies soon after an injury or early in the osteoarthritis process will assist in preventing further degenerative damage.
Dr. Stacey Guggino, ND, LAc, graduated from the National College of Natural Medicine in Portland, Oregon with a Doctorate in Naturopathy and a Master’s degree in Oriental Medicine. For the past 12 years, she has specialized in treating pain and sports injuries with acupuncture and prolotherapy. Dr. Guggino has also studied and practiced aesthetic medicine for 11 years.
Sources
- Maldonado M, Nam J. The role of changes in extracellular matrix of cartilage in the presence of inflammation on the pathology of osteoarthritis. Biomed Res Int. 2013;2013:284873. doi: 10.1155/2013/284873. Epub 2013 Aug 28. PMID: 24069595; PMCID: PMC3771246.
- C. Rosalia Costa, William B. Morrison, and John A. Carrino. Medial Meniscus Extrusion on Knee MRI: Is Extent Associated with Severity of Degeneration or Type of Tear? Musculoskeletal Imaging July 2004. Volume 183, Issue 1.
- Daszkiewicz K, Łuczkiewicz P. Biomechanics of the medial meniscus in the osteoarthritic knee joint. PeerJ. 2021 Nov 24;9:e12509. doi: 10.7717/peerj.12509. PMID: 34900428; PMCID: PMC8627128.



