For many individuals, a cough, a sneeze or laugh produces more than the expected sound. Some people require daily preparations to avoid embarrassment or preoccupation. This occurrence is urinary incontinence, or urinary leakage. This condition can progress gradually or present episodically. Unfortunately, it can also suddenly and dramatically worsen.
It is estimated that nearly 60% of women in the United States have varying degrees of stress incontinence.1
There are four forms of incontinence:
- Stress Incontinence describes the condition where force from a sneeze or cough produces urine
- Urgency Incontinence is characterized by a sudden urge to urinate
- Overactive Bladder involves the sensation of incomplete urination
- Mixed Incontinence involving the presence of multiple forms heretofore described.
Women are more affected than men and older women are more affected than younger women. Obesity, multiple pregnancies, vaginal births and nerve damage are risk factors for developing urinary incontinence. Smoking, alcohol and caffeine can worsen symptoms while pelvic floor exercises can improve symptoms.
The muscles, collectively known as the levator ani, the sphincter of the urethra and the branches of the pudendal nerve are the anatomical areas that are responsible for urinary incontinence. Depending on the severity of an individual’s case, surgery may become necessary. However, most individuals deal with symptoms classified as mild to moderate and are left on their own to deal with these uncomfortable occurrences. Tricyclic antidepressants, medications known as anticholinergics, electrostimulation and physical therapy are common forms of conventional treatment.
Often utilized in orthopedic and other treatments, Platelet rich plasma (PRP) can regenerate tissue through the presence of growth factors and cytokines, or immune regulating protrins. In the last several years this potent regenerative matrix has been applied to the urogenital area for the promotion of improved sexual health and incontinence. The growth factors assist with increased vascularity and blood flow to the penis, clitoris and vagina. The increased blood flow results in a positive effect on sexual stimulation and lubrication. These same growth factors applied to areas around the urethra have been shown to increase blood flow and heal damaged tissue, restoring the urethral sphincter’s function. A study published in 2021 highlighted the success of this treatment with decreased symptoms for thirteen months.2 Results varied from complete dryness following the injections to significant reduction in urinary leakage, illustrating a 60% efficacy amongst the participants.2 Individuals who did not experience improvement were those affected with neurogenic, or nerve damage incontinence.
A more recent 2024 study with sixty participants compared peri-urethral PRP combined with pelvic floor muscle training (PFMT) with that of pelvic floor muscle training PFMT alone. 90% of the participants in the PRP + PFMT arm of the study had a 50% reduction in urinary leakage while only 14% PFMT only achieved comparable results.3
The social stigma of urinary incontinence has been associated with depression, anxiety, isolation and fear in affected individuals. As a result, sexuality and general sociability are reduced due to the shame and embarrassment individuals experience.4 Empowering individuals to overcome their incontinence extends beyond urinary health alone, with rippling effects enhancing patients’ general well-being.
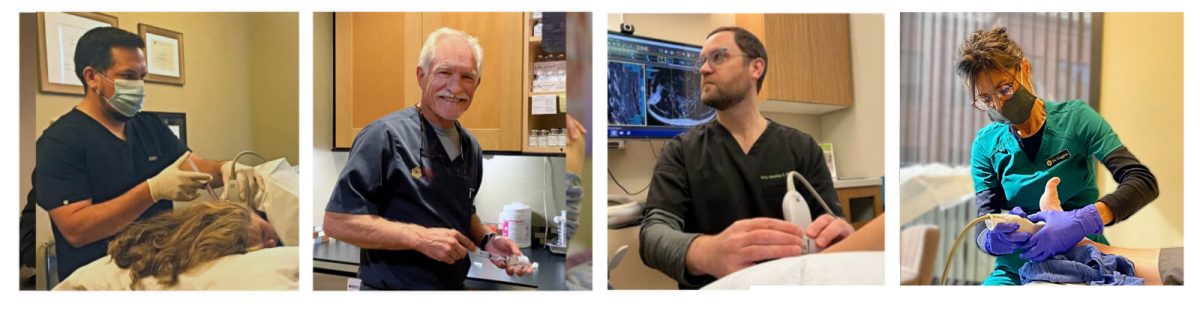
Oregon Regenerative Medicine has been providing platelet rich plasma therapies for twenty years. PRP regenerative therapy assists patients with arthritic conditions, ligament laxity, tendon and fibrocartilage tears, dry eye, traumatic brain injury, sexual health, urinary incontinence and chronic obstructive pulmonary disease among other benefits. Our primary goal is to offer therapies that harness your body’s capacity to repair and restore health to achieve optimum vitality.
Dr. Stacey Guggino, ND, LAc, graduated from the National College of Natural Medicine in Portland, Oregon with a Doctorate in Naturopathy and a master’s degree in Oriental Medicine. For the past 12 years, she has specialized in treating pain and sports injuries with acupuncture and prolotherapy. Dr. Guggino has also studied and practiced aesthetic medicine for 11 years.
Sources
- Patel UJ, Godecker AL, Giles DL, Brown HW. Updated Prevalence of Urinary Incontinence in Women: 2015-2018 National Population-Based Survey Data. Female Pelvic Med Reconstr Surg. 2022 Apr 1;28(4):181-187.
- Jiang YH, Lee PJ, Kuo HC. Therapeutic Efficacy of Urethral Sphincter Injections of Platelet-Rich Plasma for the Treatment of Stress Urinary Incontinence due to Intrinsic Sphincter Deficiency: A Proof-of-Concept Clinical Trial. Int Neurourol J. 2021 Mar;25(1):51-58.
- Saraluck A, Chinthakanan O, Kijmanawat A, Aimjirakul K, Wattanayingcharoenchai R, Manonai J. Autologous platelet rich plasma (A-PRP) combined with pelvic floor muscle training for the treatment of female stress urinary incontinence (SUI): A randomized control clinical trial. Neurourol Urodyn. 2024 Feb;43(2):342-353.
- Elstad EA, Taubenberger SP, Botelho EM, Tennstedt SL. Beyond incontinence: the stigma of other urinary symptoms. J Adv Nurs. 2010 Nov;66(11):2460-70.
Image by Bianca VanDijk on Pixabay