Ehlers-Danlos Syndrome and Joint Hypermobility Syndrome (EDS/JHS) affects 1 in 5,000 people in the US. The condition is either inherited from a parent or caused by a genetic mutation. The hallmark traits of this affliction are connective tissue abnormalities or defects in the proteins that make up collagen. As a result, EDS/JHS individuals have ligament laxity, or looseness, and their ligament quality is more elastic. They also sometimes experience looser, more elastic skin depending on severity. In addition, because this type of connective tissue is found in the veins and arteries of our major organs, individuals with EDS may also have vascular problems1.
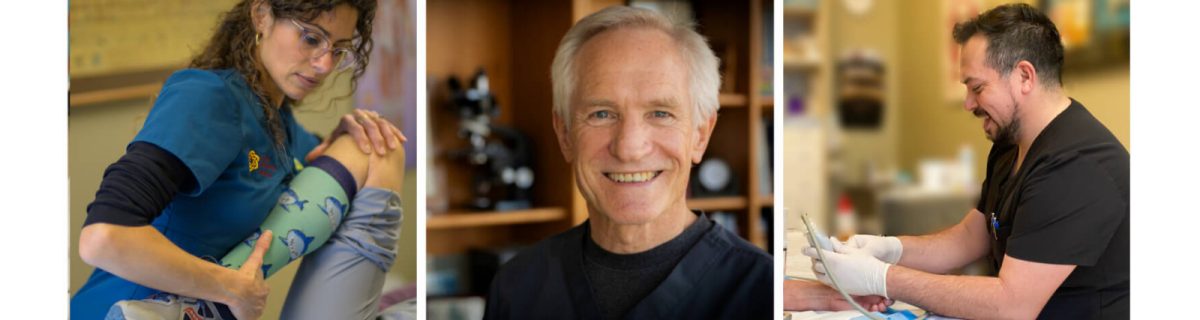
In this article, we discuss why prolotherapy is an excellent treatment intervention to assist people with EDS/JHS. In the nearly 30 years Oregon Regenerative Medicine has been performing prolotherapy, we have frequently witnessed how this treatment benefits individuals with EDS/JHS.
Ehlers- Danlos Syndrome / Joint Hypermobility Syndrome
As a result of the abnormal matrix of their collagen, individuals afflicted with EDS/JHS have more elastic, weaker ligaments. The abnormal collagen also affects the composition of muscle tendons as well 1, 2. Consequently, the ligaments and tendons are not tight or stiff enough to keep bones and joints properly positioned. The joint moves around much more liberally than it should. This can occur in all body joints in an EDS/JHS individual, depending on the severity of their condition.
The Biotensegrity Model
Biomechanical models have been proposed to explain how ligaments, muscles and tendons collectively contribute to the workings of our joints. According to one of these models, known as the biotensegrity model, “ligaments limit a joint’s range of motion, provide feedback to coordinate motor firing (muscle firing) patterns, while the muscles protect the ligaments from excessive tension by reflex contraction”3. In other words, the ligaments wrap tightly around a normal joint and how tight and supportive those ligaments are dictates how much a muscle in the area will have to work to maintain tension.
What happens when ligaments and their associated muscles are weakened by EDS/JHS and more elastic? Unfortunately, it creates a further weakening of all the involved joint structures which requires the recruitment of more muscle groups to further compensate for the abnormality3.
The cascade of these abnormalities causes EDS/JHS individuals to experience constant pain.
Pain from ligament weakness, pain from overuse and reliance on muscles and then pain from the degeneration of the joint due to the increased movement within that joint. Physical therapy, chiropractic adjustment, taping and bracing the joints may provide some help, but have limited potential results. Surgery has been shown to provide a small window of temporary relief, but the pain returns due to inherent elasticity in the connective tissue.
Prolotherapy
Developed in the 1930’s, Prolotherapy uses 12-50% dextrose mixed with an anesthetic injected into a ligament or muscle tendon’s enthesis. The enthesis is where ligaments and tendons attach to the bone. The dextrose has an osmotic effect dehydrating the area where the solution is injected. The dehydration process puts the area in a shock-like or injury-like state and initiates the body’s inflammatory cascade5. The inflammatory cascade is a three-part process by which cells infiltrate the affected area and release chemical messengers which then clean up and rebuild the affected area. This process takes around six weeks. The result is a stronger attachment and enlargement of the ligaments’ or muscles’ connection to the bone4. Studies have illustrated this effect through histological analysis, or cellular analysis. In a Pubmed meta-analysis research study that reviewed prolotherapy injections from 1990 to 2016, not only had there been a significant reduction of patient pain in many of the studies, but several studies revealed improved patterning of muscle tendons, new vessel development and improvement in joint flexion5
In the following video, an Ehlers-Danlos patient speaks about her life-changing results. She was treated with prolotherapy by Dr. Kristian Flores, MD, ND.
Prolotherapy for Ehlers-Danlos & Joint Hypermobility Research
Dr. Ross Hauser is a medical doctor who studied with Dr. Gustav Hemwall, a main contributor to the current prolotherapy technique. Dr. Hauser joined Dr. Hemwall’s practice in 1993 and the practice specializes in prolotherapy. In 2009-2010, EDS/JHS affected patients represented 8% of Dr. Hauser’s practice. In his 2011 article, Treatment of Joint Hypermobility Syndrome, Including Ehlers-Danlos Syndrome, with Hackett-Hemwall Prolotherapy1, Dr. Hauser provides case studies of the patients he treated with prolotherapy. The case studies provide a window into the complexity of these cases, his treatment protocol and the the length of time the patients experienced improvement following a series of prolotherapy treatments. Dr. Hauser mentions that, due to the severity of an affected joint, multiple injections are often required.
Prolotherapy and TMJ hypermobility
An example of the effectiveness of repeated injections can be seen in a 2017 study of twenty-three patients with hypermobility of the jaw. These patients were treated with 25% dextrose, six of them requiring 1 injection, ten requiring 2 injections and seven requiring 3 injections. Twenty-one of the twenty-three patients had statistical improvement. The improvement was in the fibrosis, or wound healing, and reducing overextension of the treated jaw joint. The proliferation of new tissue in the area prevented the joint from dislocating, which is a common occurrence with jaw hypermobility6. These patients were followed for over thirteen months and sustained continued improvement in that time. While these patients were not affected with EDS-JHS, the study illustrates the action mechanism prolotherapy has in a hypermobile joint.
We have examined the effectiveness of dextrose prolotherapy in providing healing relief for EDS/JHS individuals. PRP prolotherapy is yet another therapeutic injection that can provide even more robust healing of lax ligament and muscle tendons7. The process involves an individual’s own platelets, containing growth factors and chemical messengers enabling a strong healing cascade. The efficacy timeframe is the same with PRP prolotherapy as with dextrose and is used as an alternative therapy to dextrose.
Prolotherapy is an extremely encouraging treatment for EDS/JHS individuals where other treatment modalities have failed them. Prolotherapy is inexpensive, safe and has minimal side effects and downtime. At Oregon Regenerative Medicine, we have been able to provide pain relief in individuals that have experienced years of pain and joint dysfunction thereby significantly improving their quality of life.
Dr. Stacey Guggino, ND, LAc graduated from the National College of Natural Medicine in Portland, Oregon with a Doctorate in Naturopathy and a Master’s degree in Oriental Medicine. For the past 12 years, she has specialized in treating pain and sports injuries with acupuncture and prolotherapy. Dr. Guggino has also studied and practiced aesthetic medicine for 11 years.
Sources
- Treatment of Joint Hypermobility Syndrome, Including Ehlers-Danlos Syndrome, with Hackett-Hemwall Prolotherapy. Ross A. Hauser, MD & Hilary J. Phillips. Journal of Prolotherapy, vol 3, issue 2 May 2011; pg 612-629.
- Muscle–Tendon Tissue Properties in the Hypermobility Type of Ehlers-Danlos Syndrome.
- Rombaut, L., Malfait, F., De Wandele, I., Mahieu, N., Thijs, Y., Segers, P., De Paepe, A. and Calders, P.Arthritis Care Res, 64: 2012, pg 766-772.
- Principles of Prolotherapy. Ravin, Cantieri, Pasquarello.American Academy of Musculoskeletal Medicine. 2008.
- A Rational for Prolotherapy. Allen R. Banks Ph.D. Journal of Orthopaedic Medicine Vol 13 1991 No 3
- A Systematic Review of Dextrose Prolotherapy for Chronic Musculoskeletal Pain. Clin Med Insights Arthritis Musculoskelet Disord. 2016; 9: 139–159.
- Single Injection Technique Prolotherapy for Hypermobility Disorders of TMJ Using 25 % Dextrose: A Clinical Study. J Maxillofac Oral Surg. 2017 Jun; 16(2): 226–230.Comparison of Platelet Rich Plasma and Prolotherapy in the Management of Osteochondral Lesions of the Talus: A Retrospective Cohort Study. Med Sci Monit. 2019 Jul 30;25:5640-5647. doi: 10.12659/MSM.914111.