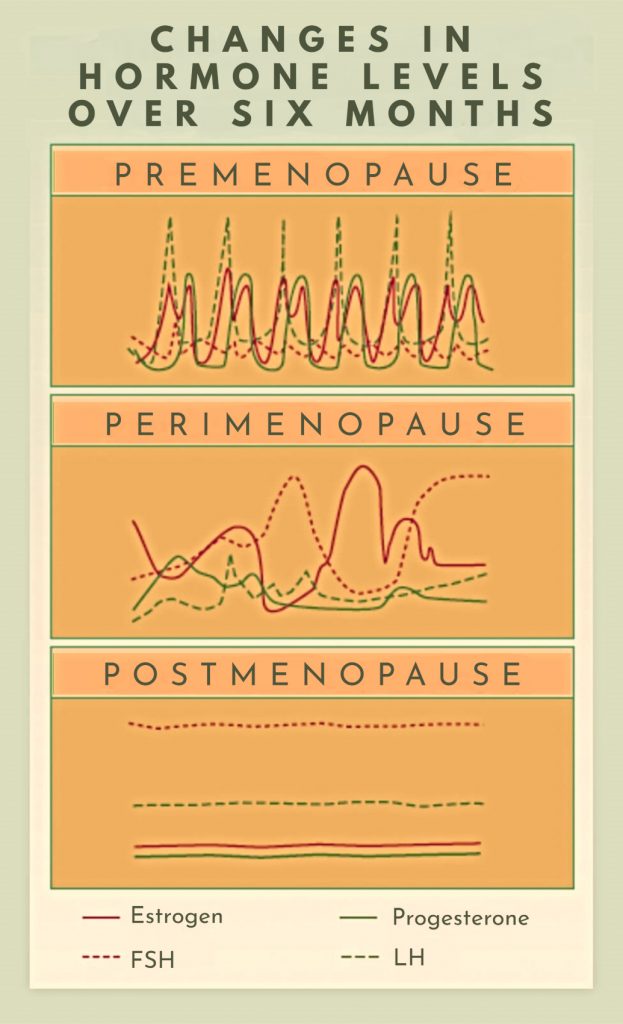
Stages of Menopause
If you’re a female in your forties and start to experience symptoms like hot flashes or irregular menstrual cycles, you may be in the hormonal transition phase we call perimenopause. (“Peri” means near or around.) On average, perimenopause lasts between 2-10 years. Then, after 12 months without a menstrual cycle, you are officially through menopause and into the postmenopausal phase. Knowing the stage you’re in is helpful in hormone replacement therapy. We alleviate symptoms associated with each phase differently.
Hormonal Changes in Each Stage of Menopause
During the menstrual years, a healthy cycle reflects a consistent, repetitive pattern of hormonal changes every month. Then, during the perimenopause phase, hormones become more volatile – the rhythmic pattern is lost, and we see symptoms associated with irregular surging of estrogen and progesterone, like hot flashes, irregular cycles, difficulty sleeping, mood disorders, change in libido, brain fog and increased aches/pains. Then in the postmenopausal phase, the hormones start to flatline, and you may experience symptoms related to estrogen deficiency, like vaginal dryness, thinning skin and hair, bone loss, and changes in your metabolic health.
Supportive Treatments for Menopause:
The treatments of symptoms in perimenopause are different than the postmenopausal phase. During perimenopause, I rely heavily on what can balance or modulate the hormonal fluctuations, like oral micronized progesterone and phytoestrogens. Additionally, any added stress to your system, like blood sugar imbalance, nutritional deficiencies, thyroid disease, cortisol irregularity, and digestive distress, can further exacerbate your symptoms. So, we really need to create a holistic approach. When you are officially in the postmenopausal phase, we may consider hormone replacement therapy (HRT) with estrogen, progesterone, testosterone and DHEA.
Hormone Replacement Therapy for Menopause Treatment:
There is a lot of misinformation around hormone replacement therapy, so let me offer some insight.
First, there are 3 types of “estrogen” products available:
- Ethinyl estrogen (EE), used in birth control
- Conjugated equine estrogen (CEE, aka Premarin), a synthetic estrogen used mostly in menopause
- Estradiol (E2) and Estriol (E3), which are biologically identical to the compounds produced by your ovaries.
There are bio-identical options readily available in commercially available products that you can pick up at any pharmacy, rather than needing a compounded formula.
For “progesterone”, there are 3 types:
- Various synthetic progestins used in birth control pills
- Medroxyprogesterone acetate (MPA, aka Provera), used in birth control and menopause
- Oral micronized progesterone (OMP), a bioidentical compound, available in 100mg or 200mg capsules.
Current research suggests transdermal estradiol (E2 patch) paired with oral micronized progesterone (OMP) has the lowest risk profile of any combination of HRT, is effective at reducing symptoms related to the hormonal changes of menopause, and even prevents ailments associated to a hormone deficiency state, like osteoporosis and urogenital (aka pelvic) pain and dysfunction. This is important to note, as we commonly hear about negative side effects of hormone replacement therapy. However, these findings are often associated with synthetic preparations like oral CEE and MPA, NOT the bioidentical options. So, when considering hormone replacement therapy, know the details of your regimen, because not all treatments are the same.
Individualized Menopause Treatment
Supportive care during menopausal changes is not a one-size-fits-all type of protocol. Since your symptoms may be different than other women, there are many details to consider. If you want to discuss which options are best for you, call our office to schedule a visit with me, Dr. Michelle Young, and we can create a plan that gets you back to feeling like yourself.
Sources
Borda LJ, Wong LL, Tosti A. Bioidentical hormone therapy in menopause: relevance in dermatology. Dermatol Online J. 2019 Jan 15;25(1):13030/qt4c20m28z. PMID: 30710894.
Mirkin S. Evidence on the use of progesterone in menopausal hormone therapy. Climacteric. 2018 Aug;21(4):346-354. doi: 10.1080/13697137.2018.1455657. Epub 2018 Apr 9. PMID: 29630427.
Notelovitz M. Clinical opinion: the biologic and pharmacologic principles of estrogen therapy for symptomatic menopause. MedGenMed. 2006;8(1):85. Published 2006 Mar 28.
Harman SM, et al. Arterial imaging outcomes and cardiovascular risk factors in recently menopausal women: a randomized trial. Ann Intern Med. 2014 Aug 19;161(4):249-60. doi: 10.7326/M14-0353. PMID: 25069991.
Stute P, Neulen J, Wildt L. The impact of micronized progesterone on the endometrium: a systematic review. Climacteric. 2016 Aug;19(4):316-28. doi: 10.1080/13697137.2016.1187123. Epub 2016 Jun 9. PMID: 27277331.
Effects of hormone replacement therapy on endometrial histology in postmenopausal women. The Postmenopausal Estrogen/Progestin Interventions (PEPI) Trial. The Writing Group for the PEPI Trial. JAMA. 1996 Feb 7;275(5):370-5. doi: 10.1001/jama.1996.03530290040035. PMID: 8569016.
Photo by Engin Akyurt on Unsplash