Knee meniscus tears are a conundrum for conventional medicine. That’s because surgery actually does not repair the meniscus, surgery just means removing a portion of the meniscus. And removing the damaged meniscus means removing the cushion that protects the cartilage covering the femur and the tibia. The result is a loss of the protective cartilage and the eventual worsening to bone-on-bone arthritis of the knee. In fact, the American College of Sports Medicine recommends against surgery for meniscus tears because it is often ineffective in relieving pain and, even more important, meniscus surgery triples your risk of a knee replacement later in life.1
When patients come to see us for knee pain, they often present with a very common issue: nagging, up-and-down knee pain/swelling, and/or knee instability that has become increasingly worse over the last few months or years and now is interfering with descending stairs and full participation in exercise. They often recall a recent minor injury, or even a past history of injury in their 20s or 30s that resolved gradually shortly after.
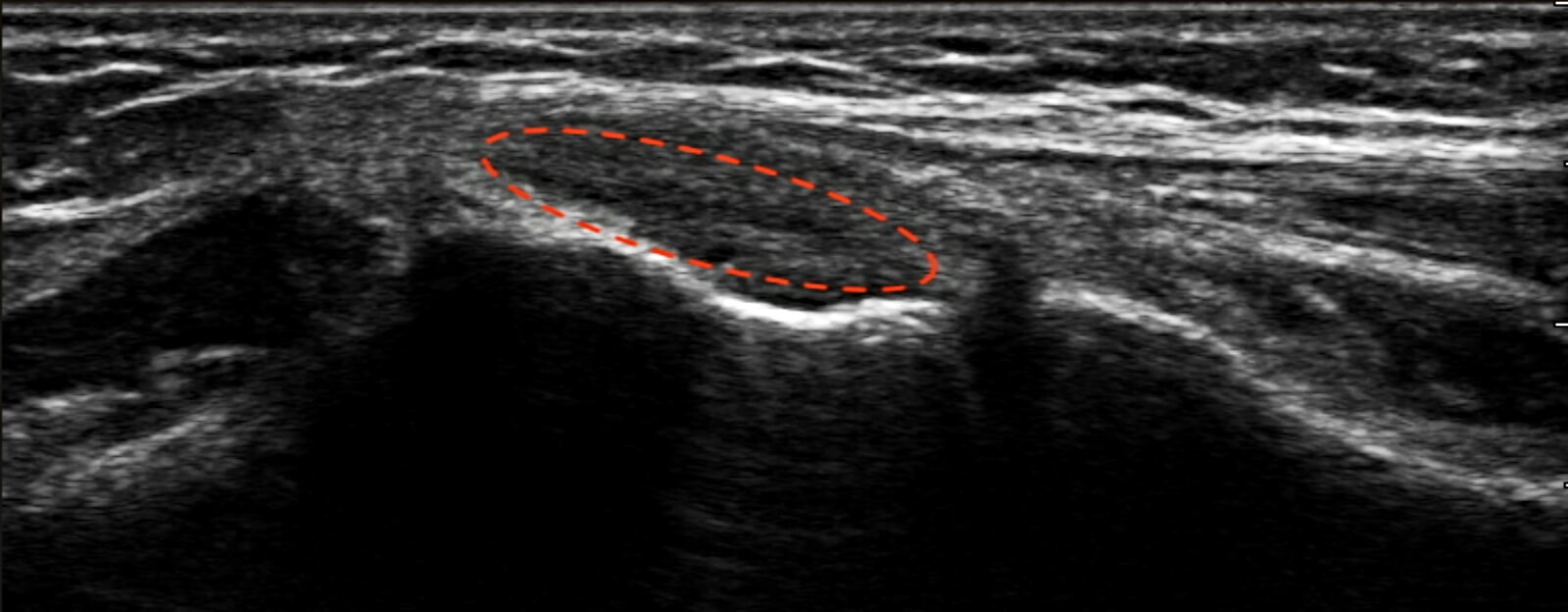
Using in-office high resolution ultrasound, we are able to image tears and degenerative changes to the meniscus with greater resolution than can be seen with an expensive MRI. In fact, ultrasound provides a clear, easy to visualize dynamic image that the patient can see in real-time for themselves. With proper diagnosis, we know the cause of our patient’s pain or instability.
This is where autologous biocellular adipose graft therapy (“stem cell therapy”) really shines. By creating a powerful healing response that can modulate inflammation and repair damaged tissue, adipose graft therapy is an excellent therapy for meniscus tears.

The average patient presenting with meniscus tears will respond very well to stem cell treatment. Performed under ultrasound guidance and local anesthetics, the regenerative medicine is placed exactly into the areas that need healing and the mixture of mesenchymal stem cells and growth factors begin to do their work. With the guidance of our physical therapist, a gradual succession of exercises are begun. After 1 month, most have mild improvement and after 3 months most return to full activities with mild limitations. Depending on the overall health of their knee, healing will continue for about 8-12 months before full resolution.
The current scientific literature shows immense promise for meniscus tears. In a 2021 study of 20 patients with meniscus tears and osteoarthritis who had all failed conservative therapy (physical therapy), adipose therapy provided a greater than 60% reduction in pain, better knee function, and did so for over a year with a single treatment.2
Our patients at ORM see much better than 60% improvement for patients who don’t wait for years to do something about their pain. Meniscus tears in younger patients without osteoarthritis do extraordinarily well and reach complete healing without limitations. Studies showing proof-of-concept for adipose therapy actually repairing tears and increasing meniscal tissue volume continue to be published.3,4,5,6
Both traumatic tears and degenerative tears of the meniscus are very common and can come from old injuries or new activities. Any twisting, pivoting, or planting of the legs can result in even minor injuries causing pain. Don’t fall into the trap of thinking that physical therapy and surgery are your only options for meniscus tears. Utilize your body’s own healing power and stay active.
Dr. Noel Peterson, ND, DAAPM, is the Medical Director of Oregon Regenerative Medicine, and has practiced naturopathic medicine in Lake Oswego, OR, since 1978. He specializes in natural and regenerative cellular medicine, including Prolotherapy, PRP (Platelet Rich Plasma), and Autologous Stem Cell therapy. Peterson has taught prolotherapy nationally and internationally. In 2019, the Oregon Director Association of Naturopathic Physicians (OANP) and National University of Natural Medicine (NUNM) selected Dr. Peterson to be honored with naturopathic medicine’s prestigious Living Legend Award.
Sources
- Rongen JJ, Rovers MM, van Tienen TG, Buma P, Hannink G. Increased risk for knee replacement surgery after arthroscopic surgery for degenerative meniscal tears: a multi-center longitudinal observational study using data from the osteoarthritis initiative. Osteoarthritis Cartilage. 2017;25(1):23-29.
- Malanga GA, Chirichella PS, Hogaboom NS, Capella T. Clinical evaluation of micro-fragmented adipose tissue as a treatment option for patients with meniscus tears with osteoarthritis: a prospective pilot study. Int Orthop. 2021;45(2):473-480.
- Centeno CJ, Busse D, Kisiday J, Keohan C, Freeman M, Karli D. Regeneration of meniscus cartilage in a knee treated with percutaneously implanted autologous mesenchymal stem cells. Med Hypotheses. 2008;71(6):900-908.
- Pak J, Lee JH, Lee SH. Regenerative repair of damaged meniscus with autologous adipose tissue-derived stem cells. Biomed Res Int. 2014;2014:436029.
- Mahajan PV, Subramanian S, Parab SC, Mahajan S. Autologous minimally invasive cell-based therapy for meniscal and anterior cruciate ligament regeneration. Case Rep Orthop. 2021;2021:6614232.
- Onoi Y, Hiranaka T, Nishida R, et al. Second-look arthroscopic findings of cartilage and meniscus repair after injection of adipose-derived regenerative cells in knee osteoarthrits: Report of two cases. Regen Ther. 2019;11:212-216.