So much weight loss media attention has been directed towards Ozempic, Mounjaro, Tirzepatide, Wegovy, Zepbund or Semaglutide that it is hard to keep all the facts straight about these GLP-1 agonist hormones. In this article, we will be diving into what GLP-1 agonists are, what they do in the body and their potential for beneficial use.
What is a GLP-1 agonist?
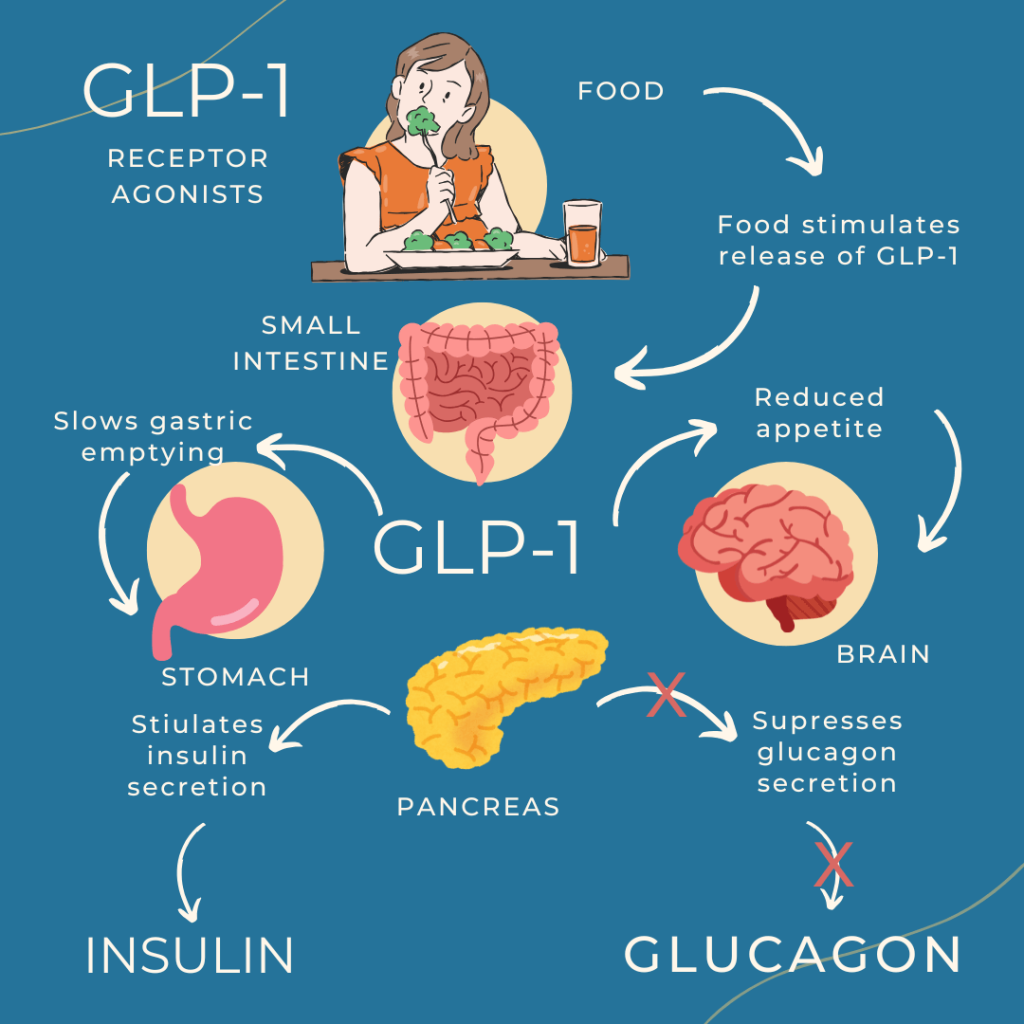
GLP-1 or glucagon-like peptide 1, are hormones that are released in the lower intestine. The GLP-1 hormone receptor, or the place where the hormone connects and initially acts upon, is in the pancreas. Within 10-15 minutes of a meal, GLP-1 is released by cells in the intestinal lining and travels through the bloodstream to the pancreas, where it attaches to receptors that have the following effects.The GLP-1 hormone first shuts down glucagon release, or the body’s way of producing its own glucose, and it signals the body to produce insulin, which drives the glucose from the bloodstream into the cells. The GLP-1 hormone also slows gastric emptying, regulating how much glucose the body absorbs from food. The GLP-1 also creates satiety (or a feeling of fullness) through stimulating neurons in the brain center.1In essence, this little hormone has a lot of responsibilities (Fig 1).
Why is this hormone deficient in some people? Interestingly, the foods that are most responsible for stimulating the natural production of GLP-1 in our intestines are high fiber foods. Foods such as whole, sprouted grains, legumes, eggs, olive oil, nuts, and avocado. GLP-1 deficiency arises when the diet consists largely of fast carbohydrates, such as crackers, chips, white breads and foods with high amounts of fructose. High fiber foods feed the microbiota, or the bacteria populating the large intestine. The healthy gut microbiota ferments the fiber to produce short chain fatty acids, SCFA’s. These SCFA’s promote the production of GLP-1 in the intestine. Individuals struggling with Type 2 diabetes and obesity tend to have an imbalance in their intestinal bacteria producing an unhealthy microbiota.2
This leads to a lack of the bacteria that ferments SCFA’s, thus reducing GLP-1 production.3
A bit of history
In the mid 1980’s researchers discovered high concentrations of GLP-1 in subjects’ intestinal lining. The researchers observed that in the presence of a large oral dose of glucose, GLP-1 was released from cells stimulating the release of insulin from the pancreas which in turn reduced blood sugar. However, they also discovered a limitation of naturally produced human GLP-1. It only lasts for 1-2 minutes in the body.
Concurrently, another researcher had found a homolog, or structurally similar, GLP-1 in the Gila monster, a venomous lizard indigenous to the southwest. The Gila monster’s GLP-1 lasted for two hours in the body. Researchers then experimented with hundreds of different combinations of compounds such as fatty acids and amino acids to link to the GLP-1 to make it more stable and last for a longer time in the body. The result? A product from Novo Nordisk that has a half-life, or a medication that stays at a therapeutic level, for 7 days! This means that this medication only needs to be administered once a week. In 2005, the FDA cleared the first GLP-1 agonist to be used with Type 2 diabetic patients. In 2017, the FDA cleared Ozempic to be used in patients with Type 2 diabetics. In 2021, Wegovy was cleared to be used in patients for weight loss.
GLP-1 agonist limitations for weight loss
The benefits of a GLP-1 agonist: the satiety, managed blood sugar, slowing gastric emptying- only occur while taking the medication. If someone goes off the medication, those benefits cease. There is also a plateauing of weight loss that occurs around 60 weeks of administration. This means that the weight loss that occurred in the first 12 months will be the extent of total weight loss. Continued administration of the medication is necessary to maintain what has been lost. GLP-1 side effects are also considerations. Nausea, vomiting, abdominal pain, diarrhea and constipation are the most common side effects individuals experience while taking a GLP-1 agonist. The intensity of the nausea can be such a deterrent that many patients stop taking the medication.
What about microdosing a GLP-1 agonist?
Within the last several years, clinicians have been experimenting with different ways to dose the GLP-1 agonists. Rather than provide the full dose of the medication, which can be taken orally or via an injection, the dosage remains much lower for the duration of use. Despite the micro-dosage, patients are achieving the benefits of the full dose without significant side effects. Some clinicians are using the microdose amount for maintenance after the highest weight loss has been achieved.
Opinions
My thought on the GLP-1 agonists is that it should be used as a tool rather than an ultimate solution. In other words, using the medication to feel satiated with smaller portion sizes is a way to train the body to achieve a new set point of hunger and metabolism. Incorporating foods that are known to naturally stimulate GLP-1 while also exercising to build muscle is a healthy strategy either with or without the medication. I feel that regular monitoring of body systems such as liver, kidneys, red and white blood cells and thyroid should be performed. Additionally, having a provider to support you with well-known strategies to reduce the side effects enables an easier commitment for long term use of the medication. If you have questions or if you are curious whether a semaglutide is a good fit for you, contact your provider.
Dr. Stacey Guggino, ND, LAc, graduated from the National College of Natural Medicine in Portland, Oregon with a Doctorate in Naturopathy and a master’s degree in Oriental Medicine. For the past 12 years, she has specialized in treating pain and sports injuries with acupuncture and prolotherapy. Dr. Guggino has also studied and practiced aesthetic medicine for 11 years.
Sources
-
- Liu QK. Mechanisms of action and therapeutic applications of GLP-1 and dual GIP/GLP-1 receptor agonists. Front Endocrinol (Lausanne). 2024 Jul 24;15:1431292. doi: 10.3389/fendo.2024.1431292.
-
- Hinnen D. Glucagon-Like Peptide 1 Receptor Agonists for Type 2 Diabetes. Diabetes Spectr. 2017 Aug;30(3):202-210. doi: 10.2337/ds16-0026. PMID: 28848315; PMCID: PMC5556578.
-
- Zeng Y, Wu Y, Zhang Q, Xiao X. Crosstalk between glucagon-like peptide 1 and gut microbiota in metabolic diseases. mBio. 2024 Jan 16;15(1):e0203223. doi: 10.1128/mbio.02032-23. Epub 2023 Dec 6.
Photo by I. Yunmai on Unsplash



