As we age, the ability of our bodies to produce choline declines. Choline is a nutrient that is responsible for memory, mood and muscle control. It assists with fat metabolism, is a methyl donor and lipoprotein transporter.1,2 It is produced by the liver as well as contained in some foods we eat (Fig 1). The synthesis, or production of choline, from our liver is said to account for only 20-30% of the choline our bodies need. Therefore, it is necessary for additional sources to be obtained through diet or supplementation.
Men and postmenopausal women have a higher need for Choline supplementation. PEMT, or phosphatidylethanolamine N-methyltransferase, is a gene that encodes the enzyme to produce choline/phosphatidylcholine (a form of choline) in the liver. PEMT is affected by estrogen. Less estrogen reduces the signaling of the PEMT gene in the liver to produce choline. Thus, postmenopausal women and men are more susceptible to choline deficiencies as compared to premenopausal women due to the reduced presence of estrogen. Cycling female rats, as a comparison, are shown to have 10-50% more PEMT activity than male rats.
Another factor in Choline deficiency are SNPs or single nucleotide polymorphisms. SNPs are variations in the genetic sequencing of DNA which can increase the likelihood of developing certain diseases. Some DNA SNPs have greater disease severity than other sequences. For example, certain PEMT SNPs have a greater influence in reducing the production of choline in the liver resulting in the interruption of fat metabolism, leading to various metabolic diseases (Fig 2).
Choline Deficiency and Disease
There is a famous multigenerational study known as the Framingham Study that began in Massachusetts in 1948. The study’s focus was to investigate cardiovascular risk in one community over many years. The study is ongoing and is in its third generation. In 1991-95, the study’s researchers asked over 3200 participants to fill out questionnaires about dietary intake of 126 food items and supplements over the 12 months prior to the questionnaire. This cohort of study participants then had a neuropsychological assessment every 5-6 years thereafter. From this data, the researchers deduced that there was a significant associative risk of developing dementia or Alzheimer’s disease with a diet low in choline.2
To assess genetic variation influencing choline production, a 2023 study looked at the various PEMT SNPs among older males and females.3 The study revealed that certain SNPs were more impactful than others in developing liver or cardiovascular disease. In this study, the GG PEMT SNP was associated with greater risk of developing fatty liver disease in a Taiwanese study population. The investigators observed that the GG SNP group was associated with higher triglycerides, increased body mass Index, greater insulin resistance, increased low-density lipoproteins (LDLs, or bad cholesterol) and reduced high-density lipoproteins (HDLs, or good cholesterol). The investigators noted that women who had a diet consisting of 448 mg of choline daily had reduced risk factors with better LDL, insulin resistance and triglyceride tests. Men with the GG PEMT SNP, on the other hand had a 3.5-fold greater risk of developing cardiovascular disease with greater than 448 mg of dietary choline daily.
Why this difference between men and women? Even with adjustments to the data to make a more even comparison (for body mass index and HDLs), the men were still shown to have greater metabolic stress, greater insulin resistance and reduced good HDL cholesterol with this GG PEMT SNP. HDLs are generally higher in women because of the presence of estrogen. Women had elevated HDLs with the choline diet while men did not. HDL, or good cholesterol, takes cholesterol from the bloodstream to be reprocessed by the liver and eliminated from the body. Another likely reason for the increased cardiovascular risk is due to the choline itself. Too much choline can increase an enzyme known as TMAO, or trimethylamine-N-oxide. When intestinal cells are overloaded with choline, our gut bacteria makes TMAO. TMAO is associated with both cardiovascular risk and liver injury.
The Take-Home on Choline
The association of choline deficiency and disease cannot be overstated. Ensuring that a diet is rich in choline, and if not, supplementing with a supplement known as phosphatidylcholine is easy and affordable. If you are supplementing with choline, consult with your doctor about the appropriate dosage for your body and have your TMAO levels checked.
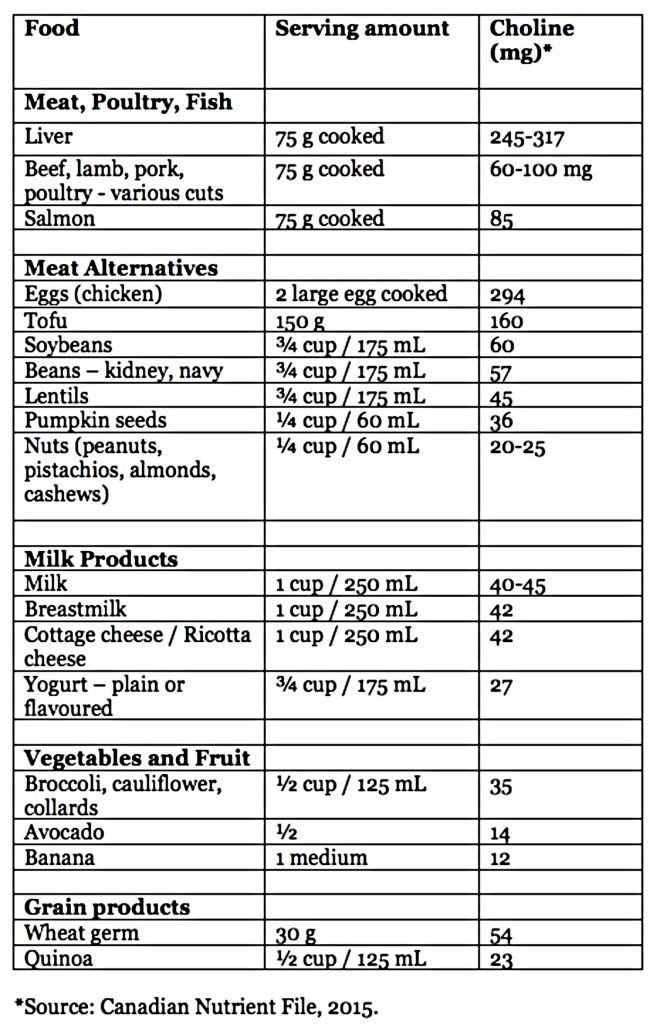
(Fig 1)
The Role of PEMT in Metabolism
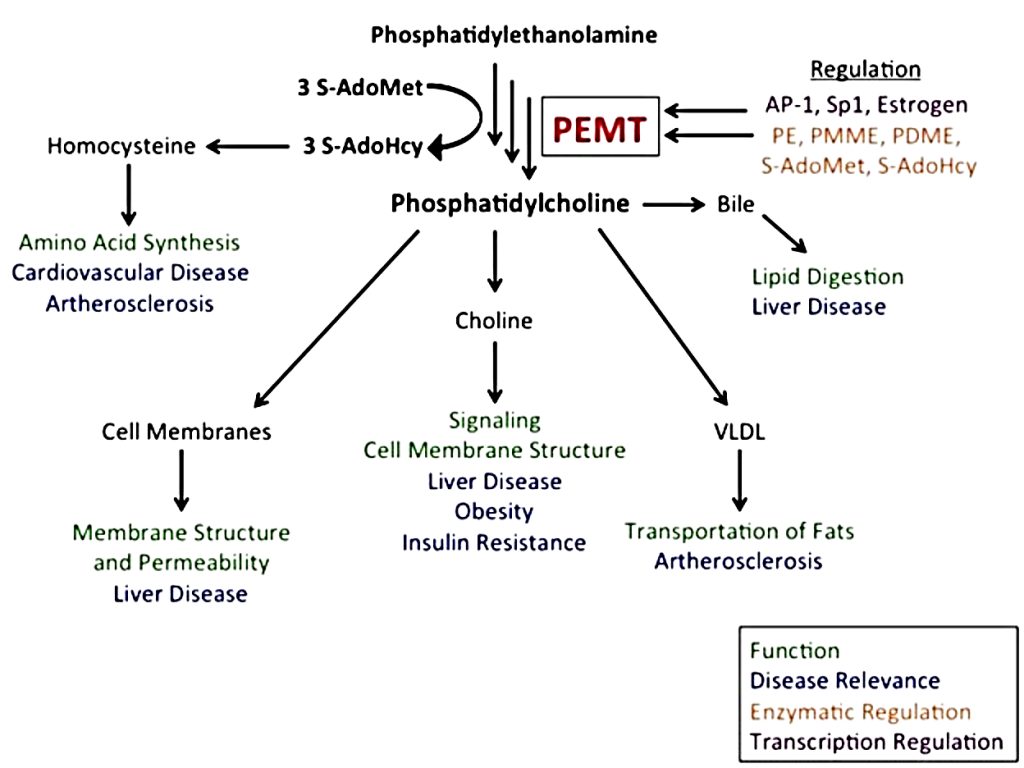
(Fig 2)
Dr. Stacey Guggino, ND, LAc, graduated from the National College of Natural Medicine in Portland, Oregon with a Doctorate in Naturopathy and a master’s degree in Oriental Medicine. For the past 12 years, she has specialized in treating pain and sports injuries with acupuncture and prolotherapy. Dr. Guggino has also studied and practiced aesthetic medicine for 11 years.
Sources
- Choline: Fact Sheet for Health Professionals, National Institute of Health: Office of Dietary Supplements, Updated: June 2, 2022
- Bekdash RA. Neuroprotective Effects of Choline and Other Methyl Donors. Nutrients. 2019;11(12):2995. Published 2019 Dec 6. doi:10.3390/nu11122995
- Wu CH, Chang TY, Chen YC, Huang RS. PEMT rs7946 Polymorphism and Sex Modify the Effect of Adequate Dietary Choline Intake on the Risk of Hepatic Steatosis in Older Patients with Metabolic Disorders. Nutrients. 2023;15(14):3211. Published 2023 Jul 19. doi:10.3390/nu15143211



