Not all tendinopathies are created equal. Some tendinopathies involve partial to full thickness tears. Others involve an intact tendon structure, but the tendon itself is thickened from persistent low-grade inflammation or recurrent injuries. Lastly, some tendinopathies include bony or calcific lesions. Whether it be an Achilles tendon, shoulder rotator cuff tendon, or common extensor tendon of the elbow (Tennis elbow); knowing the specific subtype of the tendinopathy will help choose which treatment plan is most appropriate and most likely to result in an outstanding outcome.
For tendinopathies that involve partial to full thickness tearing, microfragmented adipose tissue (MFAT) graft stem cell therapy is indicated. The physical (scaffolding and matrix) and physiologic (stem cells that can heal tissue) properties of MFAT can be employed to fill in the tendon tear and then, with time, differentiate into normal healthy tendon.
For the subtype of tendinopathies that involve tendon thickening, bony or calcific lesions, injection therapies can be helpful, but often the tendon needs to be debrided prior to injection therapy.
When a tendon has been chronically painful, what we often see is a thick tendon that has had low grade injuries and inflammation, without healing resolution. The extra thickness in the tendon is often due to fibrotic tendon tissue (think of this as scar tissue). When there is such significant scar tissue within the tendon, it interferes with the body’s attempts to heal the tendon on its own. To restore tendon health, the scar tissue first must be removed. How can this be accomplished?
Three main ways to remove tendon scar tissue
One way would be surgically. Here a surgeon will open the skin, dissect down to the tendon, then manually scrape the tendon with a scalpel or other device, hoping to remove the scar tissue. The downsides to this are that it requires an open surgical procedure which has multiple risks, but more importantly, on a macroscopic level (that is through the eyes of the surgeon) there is no definitive way to determine which part of the tendon is scar tissue (thus to be removed) and that which is healthy tendon tissue (to be left undisturbed). Therefore, surgical removal also will have collateral damage to good and healthy tendon tissue.
A second option is a procedure called needle tenotomy. Here the interventionist will use a hypodermic needle and make multiple passes through the involved tendon, hoping to break up and release the scar tissue, all the while inducing trauma to the tendon in hopes of initiating a healing response. This technique does not require a surgical incision, but it perhaps does not do as good of a job at physically breaking up or removing the scarred tendon. This technique is also nonselective for the diseased tendon tissue only.
The third way to achieve the goal of removing diseased/scarred tendon tissue is to perform a percutaneous tenotomy/debridement using a specialized needle. There are several different FDA approved percutaneous tendon debridement devices, but one that I favor is called the Tenex device.
The Tenex device is a brilliantly designed needle to accomplish debridement in a safe, effective, and complete way. The Tenex device uses two separate systems to achieve the goal of tendon debridement. First, the needle itself oscillates at a specific ultrasonic frequency. This frequency is set to break up and cut through diseased/scarred tendon tissue yet spare the healthy tendon. As this device is passed through the tendon (using ultrasound guidance), it selectively breaks down only the diseased part of the tendon. Secondly, the needle has a wash and vacuum (lavage and aspiration) technology. As the needle tip is dissolving the diseased tendon, overlying the needle is a sheath that shoots out sterile saline and then vacuums it out. So not only does this device break up the bad tendon tissue, but also it selectively removes it!
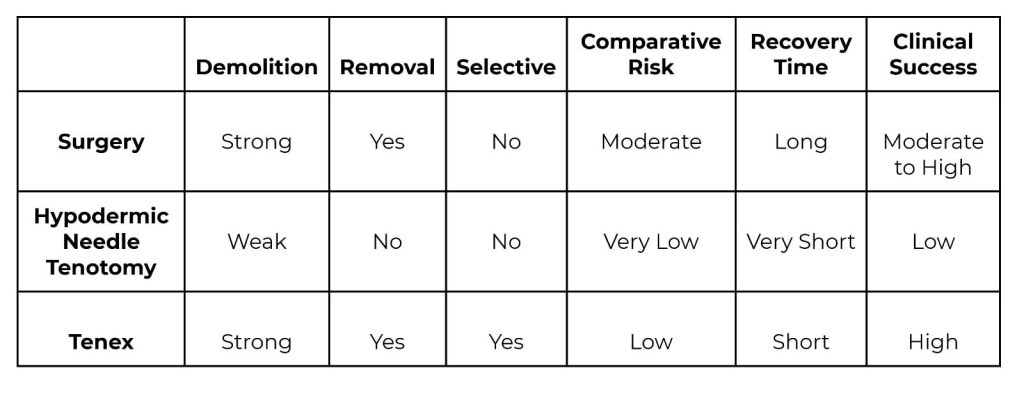
To my knowledge, the Tenex device is currently the most precise way to remove thickened, scarred, and diseased tendon tissue. The table below compares the main characteristics of the three treatment options discussed.
A good analogy for this is that of remodeling a house. If you buy a fixer upper, you don’t just start putting up new drywall over the old or on frames that have dry rot. You don’t just start updating the house, without first demolishing and removing the parts of the house that are in disrepair. The Tenex device does a great job at the demolition and removal phase of remodeling for tendon health. Yet the actual updating and remodeling still need to be accomplished. That’s why I’ll often recommend Tenex debridement but then follow it the same day with a regenerative medicine injection. Here the regenerative medicine will augment the remodeling and updating.
This is a similar philosophy when trying to treat the subtype of tendinopathies that involve bone and/or calcium deposits. Acute calcific tendinitis can be extremely painful, and the demolition and removal accomplished by the Tenex device can provide a quick and definitive treatment. Sometimes bony spurs develop where a tendon originates or inserts on a bone and sometimes these spurs can be painful. A different Tenex needle with a different ultrasonic frequency can cut through bone and wash and vacuum it out. In summary, if you are suffering from tendinopathy, you may be a good candidate for the Tenex procedure. Another condition that responds very well to Tenex is plantar fasciitis. I’ve treated many shoulder rotator cuff tendons, plantar fascias, medial and lateral epicondylitis (Golfer’s and Tennis elbow), as well as Achilles tendinopathy, heel spurs, and Haglund syndrome with great results. Inquire with our front desk about scheduling a consultation regarding this powerful treatment for tendinopathies.
Dr. Manning is recognized internationally for his expertise in diagnostic and interventional musculoskeletal ultrasound and serves as a subject matter expert in the field. Dr. Manning is president and a founding member of the Naturopathic Orthopedic Medicine Academy, board member of the Oregon Association of Naturopathic Medicine, member of the Interventional Orthobiologics Foundation, and serves on the Oregon Pain Management Commission. From professional athletes to weekend warriors or those with persistent pain, Dr. Manning delivers individualized care and exceptional outcomes. He practices at Oregon Regenerative Medicine, teaches at the National University of Natural Medicine, and trains and consults other providers at Regenerative MSK Consultants. In 2024, Dr. Manning was awarded the inaugural Rising Star Award from the Oregon Association of Naturopathic Medicine, highlighting his excellence and leadership within naturopathic medicine in the state of Oregon.



