Are more of your patients reporting injuries and pain in their feet since the COVID lockdowns? Ours certainly are. A seemingly universal effect of the COVID-19 closures has been an increase in walking and running for exercise due to closed gyms and canceled fitness classes. Plantar fasciosis and achilles tendinopathy are two of the most common “overuse” dysfunctions, but their causes are commonly misunderstood.
Keeping our patients moving should be a top priority, especially as it relates to stress relief and emotional well being. I have developed an in-depth understanding of foot function and health coming from thousands of patients and years of experience under the tutelage of both Dr. Noel Peterson, ND, DAAPM at Oregon Regenerative Medicine and Dr. Ray McClanahan, DPM at Northwest Foot & Ankle.
I bring a unique and valuable dual approach to foot health which addresses both prevention and treatment for people at any fitness level: First, a foundational preventive measure focused on foot alignment and strength. Second, utilization of regenerative injection therapies that encourage the body to heal itself. This approach can be applied to any patient with chronic or even recent-onset foot pain. It can be modified based on various factors such as foot strength, deformities, and history of supportive devices.
Alignment

Footwear can dramatically alter foot alignment, especially of the great toe. The primary problem in modern footwear design is that most shoes are not shaped like feet. Overly supportive and constrictive shoes can lead to bunions, over-pronation, osteoarthritis, poor circulation1,2 and neuromas (to name a few), as well as plantar fasciosis and achilles tendinopathy. The first step in foot health is wearing shoes that have:
- Wide toe box
- Zero drop
- Minimal external support
- Flexibility
With these shoe features, the foot achieves correct alignment, structural integrity is maintained, and foot function is optimized.
Strength
The muscles in your feet operate like any other muscle in your body: if you don’t use it, you lose it. Strengthening your feet necessitates using them and challenging them in a constructive way just like a strength training program for any other part of the body. The biggest downside to wearing overly-supportive shoes is that they deactivate the muscles in the feet that would otherwise be working. This leads to weakening of the feet over time and continued reliance on external support devices. Additional benefits include improved circulation, proprioception and ankle stability. There are numerous other patient-specific measures to aid in the transition to this type of approach. They are beyond the scope of this summary but are included in each individualized treatment plan. However, the general approach is the same: the foot is designed to support itself.
Healing
What happens when something goes wrong? Even with perfect health and strong feet, injuries can happen. This is especially true with significant increases in repetitive activities like walking and running. In addition to conservative measures, most causes of pain in the foot and ankle are effectively treated with regenerative injection therapies, especially when the underlying etiology is understood.
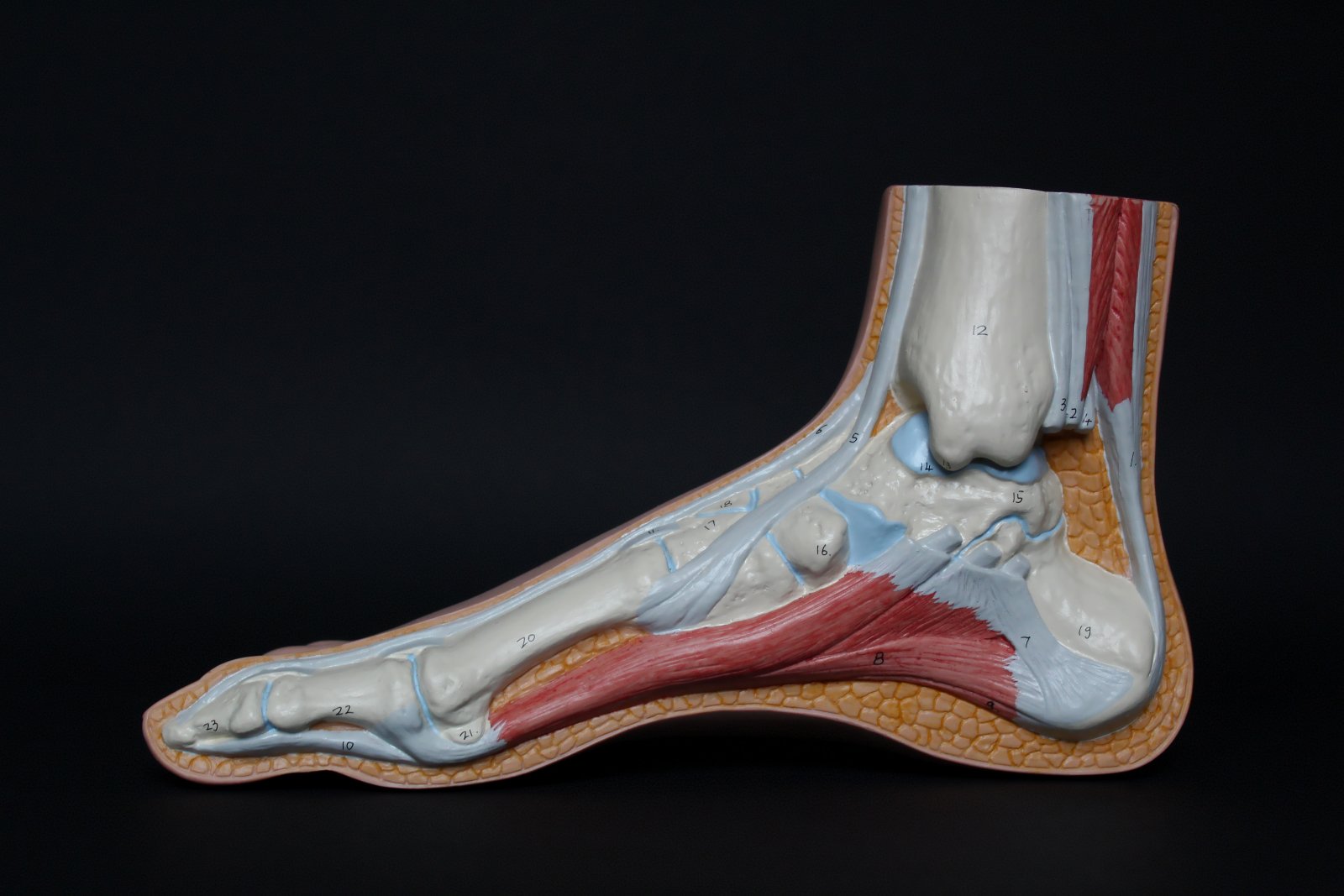
Plantar Fasciosis
The term “plantar fasciitis” is a misnomer in most cases. “-itis” refers to inflammation, and we now know the vast majority of plantar fascia pain comes not from inflammation but from degenerated tissue. Plantar fasciosis is the more correct term. Although it may seem like a superficial detail, it points to a deeper understanding of the problem: poor blood flow and cellular death3,4.
Therefore the treatment should not be focused on “limiting inflammation” with ice, steroids or NSAIDs because that’s not generally the underlying cause. Instead, promoting circulation (with proper foot alignment as discussed above) and using regenerative injection therapy are a great choice in most situations.
Mechanistically, PRP is a method of inducing a dramatic and precise increase in the circulatory elements that promote healing. The evidence bears this out:
- PRP is superior to corticosteroid injection based on AOFAS score and was far more durable, with improvements remaining at 12 months post-injection5.
- PRP is superior to kinesiotaping at 12 and 24 week follow up6.
Achilles Tendinopathy
The same “-itis” misconception applies to achilles tendinitis. In most cases histology studies show degenerative changes in the tendon, not inflammatory changes7. We know that the calcaneal insertion of the tendon has poor circulation compared to the rest of the tendon, predisposing it to over-strain injury via slower microtrauma recovery. Shortening of the gastrocnemius caused by shoes with raised heels puts excessive strain on the tendon and increases injury risk8. Excessive calcaneal movement caused by lateral heel striking and over-pronation can put undue shearing stress on the tendon and is remedied by proper footwear and alignment of the hallux.
Again, by directly addressing the degenerative process and resolving microtrauma we find similar outcomes for PRP in achilles tendinopathy:
- Leukocyte-rich PRP provides significant improvement in 2 months and is stable for over 4 years9.
- A single PRP injection improved pain and function at 3 weeks, 3 months, and 6 months. 91% of the subjects were satisfied with their treatment10.
- Injection of an adipose tissue graft showed improvement in pain and function superior to PRP and resulted in a quicker improvement11.
Regardless of where the pain is or how long standing it is, Oregon Regenerative Medicine has the holistic approach and depth of experience to get your patients back on their feet quickly and durably. We all know that with the increased stress everyone is feeling during this pandemic, regular exercise is one of the most important things your patients can do. Healthy feet lead to a healthy body, mind, and soul.
Sources
- Jacobs, J.L., Ridge, S.T., Bruening, D.A. et al. Passive hallux adduction decreases lateral plantar artery blood flow: a preliminary study of the potential influence of narrow toe box shoes. J Foot Ankle Res 12, 50 (2019).
- Wojciechowski, ND, Andrew, Importance Of Foot Circulation: Plantar Fasciosis, Varicose Veins, Correct Toes Blog, 17th July 2020.
- Lemont H, Ammirati KM, Usen N. Plantar fasciitis: a degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc. 2003;93(3):234-7.
- Wearing SC, Smeathers JE, Urry SR, Hennig EM, Hills AP. The pathomechanics of plantar fasciitis. Sports Med. 2006;36(7):585-611.
- Yang WY, Han YH, Cao XW, et al. Platelet-rich plasma as a treatment for plantar fasciitis: A meta-analysis of randomized controlled trials. Medicine (Baltimore). 2017;96(44):e8475.
- Gonnade N, Bajpayee A, Elhence A, et al. Regenerative efficacy of therapeutic quality platelet-rich plasma injections versus phonophoresis with kinesiotaping for the treatment of chronic plantar fasciitis: A prospective randomized pilot study. Asian J Transfus Sci. 2018;12(2):105-111.
- Kader D, Saxena A, Movin T, et al. Achilles tendinopathy: some aspects of basic science and clinical management. British Journal of Sports Medicine 2002;36:239-249.
- Zöllner AM, Pok JM, Mcwalter EJ, Gold GE, Kuhl E. On high heels and short muscles: a multiscale model for sarcomere loss in the gastrocnemius muscle. J Theor Biol. 2015;365:301-10.
- Filardo G, Kon E, Di Matteo B, et al. Platelet-rich plasma injections for the treatment of refractory Achilles tendinopathy: results at 4 years. Blood Transfus. 2014;12(4):533-40.
- Guelfi M, Pantalone A, Vanni D, Abate M, Guelfi MG, Salini V. Long-term beneficial effects of platelet-rich plasma for non-insertional Achilles tendinopathy. Foot Ankle Surg. 2015;21(3):178-81.
- Usuelli FG, Grassi M, Maccario C, et al. Intratendinous adipose-derived stromal vascular fraction (SVF) injection provides a safe, efficacious treatment for Achilles tendinopathy: results of a randomized controlled clinical trial at a 6-month follow-up. Knee Surg Sports Traumatol Arthrosc. 2018;26(7):2000-2010.